Treating Diabetic Retinopathy in Baltimore
Also serving Pikesville, Catonsville, Glen Burnie, & Rosedale
Developing a chronic condition like diabetes impacts your life and health. When you notice changes to your vision after a diagnosis of diabetes from your medical doctor, it may relate to the condition. Treating diabetic retinopathy requires an understanding of the underlying causes of the condition and the possible solutions that may reduce the risk of further damages to your eyes.
What is Diabetic Retinopathy?
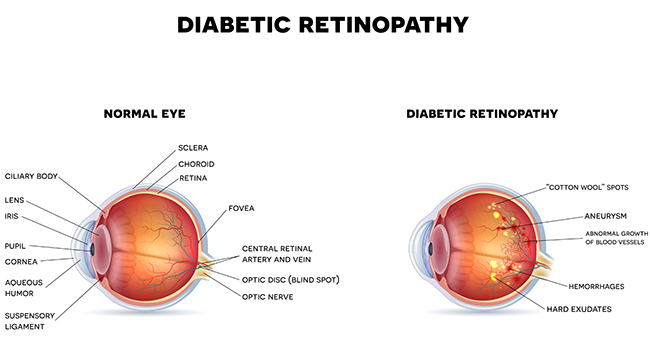
 Diabetic retinopathy is a condition related to the blood vessels in the retina. When you have high blood glucose levels, it may cause damage to the retina due to the changes in the blood vessels. Over time, you notice changes to your vision or a loss of vision.
Diabetic retinopathy is a condition related to the blood vessels in the retina. When you have high blood glucose levels, it may cause damage to the retina due to the changes in the blood vessels. Over time, you notice changes to your vision or a loss of vision.
Depending on the severity of damage to the retina, professionals at the Elman Retina Group provide treatment solutions to address the situation. We focus on the type of damage to your eyes and the possible solutions based on your situation and goals.
Impact on Your Vision
The impact of diabetic retinopathy on your vision and eyes will vary based on the severity of the situation. In early stages, we may prevent or limit vision loss by identifying the problem and taking measures to slow the progression of the condition. Unfortunately, you may not notice a problem until you begin losing your vision.
It is not possible to cure the damage to your eyes. At our clinic, we focus on slowing the progression of the condition through appropriate treatment strategies. We evaluate the severity of the damage to your retinas and then recommend a solution after determining the options for your situation. We may recommend adjustments to your normal activities as well as various corrective solutions based on your retinas and the damage to the area.
Treatment Options in Our Clinic
The treatments we offer for diabetic retinopathy depend on your needs. We may recommend surgical procedures to reduce the risk of further damages to your retina. Laser surgery may help when the damage to your retina is limited and has not yet progressed to a severe point. We may also suggest the surgical removal of the vitreous gel if you notice changes to your vision, but the retina is not damaged or has limited damages.
In certain situations, we use anti-inflammatory medications as an injection to reduce the inflammation contributing to the damages. The medication helps slow the progression of the condition when we notice inflammation during routine exams.
The key to preventing a loss of vision is regular screenings. If you have diabetes, then we recommend visiting a professional for exams at least once in six months or more regularly when we have concerns about your eyes. Early detection is the key to treating diabetic retinopathy and slowing the progression of the condition.
Diabetic Retinopathy FAQs
What are the first signs of diabetic retinopathy?
In the earliest stages, diabetic retinopathy may not cause noticeable symptoms. Over time, patients might develop blurry vision, dark spots or floaters, fluctuating sight, or difficulty distinguishing colors. Because the disease can progress silently, regular dilated eye exams are the best way to detect it before vision loss occurs.
How often should diabetics get eye exams?
Most people with diabetes should schedule a comprehensive dilated exam at least once a year. If retinopathy is present or progressing, a retina specialist may recommend visits every three to six months to closely monitor changes.
Can diabetic retinopathy be reversed?
While existing retinal damage cannot be undone, early detection and treatment can slow progression and help preserve vision. Interventions like anti-VEGF injections, laser therapy, and vitrectomy may stabilize or improve visual outcomes depending on the stage of disease.
What is the difference between proliferative and non-proliferative diabetic retinopathy?
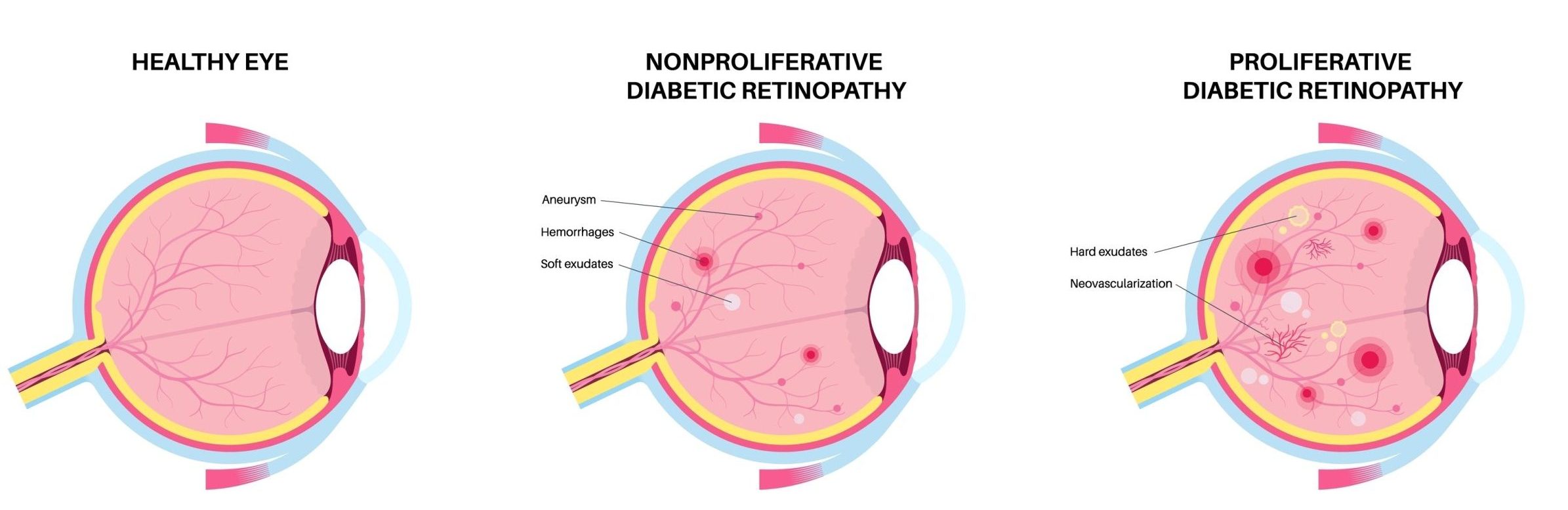 Non-proliferative diabetic retinopathy (NPDR) is the early stage, where blood vessels weaken and may leak fluid or small amounts of blood. Proliferative diabetic retinopathy (PDR) is more advanced, marked by abnormal new blood vessel growth that can scar, bleed, and even cause retinal detachment.
Non-proliferative diabetic retinopathy (NPDR) is the early stage, where blood vessels weaken and may leak fluid or small amounts of blood. Proliferative diabetic retinopathy (PDR) is more advanced, marked by abnormal new blood vessel growth that can scar, bleed, and even cause retinal detachment.
How do anti-VEGF injections work for retinopathy?
These medications block vascular endothelial growth factor, a protein that stimulates abnormal blood vessel growth. By reducing leakage and swelling in the retina, anti-VEGF injections can improve vision and limit further damage, particularly in cases of proliferative disease or diabetic macular edema.
Are laser treatments for diabetic retinopathy painful?
Laser photocoagulation is generally well tolerated. Most patients experience only mild discomfort during the procedure, which is performed in-office with local anesthetic eye drops. The goal is to seal or shrink leaking blood vessels, slowing disease progression.
What lifestyle changes help prevent diabetic eye disease?
Keeping A1C levels under control is crucial. Patients are encouraged to maintain a healthy diet, exercise regularly, quit smoking, and manage blood pressure and cholesterol. Protecting overall vascular health directly supports retinal blood vessels.
How long is recovery after a vitrectomy for retinopathy?
Vitrectomy recovery varies by patient, but most individuals resume normal activities within a few weeks. The eye may feel irritated at first, and vision improves gradually as the retina stabilizes. Follow-up visits are important to monitor healing.
Does insurance cover diabetic retinopathy treatments?
Most health insurance plans, including Medicare, provide coverage for medically necessary treatments such as injections, laser procedures, and surgery. You should verify benefits with your provider for specific details.
When should I see a retina specialist for diabetes-related vision changes?
Any new symptoms—such as blurred vision, floaters, or vision loss—warrant immediate evaluation. Even in the absence of symptoms, all diabetic patients should see a retina specialist regularly to catch changes before vision is affected.
What’s the difference between diabetic retinopathy and macular edema?
Diabetic retinopathy is the overall condition caused by long-term damage to the retina’s blood vessels from high blood sugar levels. It can progress from early non-proliferative stages to more advanced proliferative disease. Macular edema, on the other hand, is a complication of diabetic retinopathy that occurs when fluid leaks into the macula, causing swelling and blurred central vision.
Developing a chronic health condition impacts your life by causing complications in your health. When you have diabetes, you want regular screenings for diabetic retinopathy to limit possible complications. To learn more about treating retinopathy, call us today.



