Macular Edema Treatment in Baltimore
Also serving Pikesville, Catonsville, Glen Burnie, & Rosedale
While macular degeneration may be the most infamous macular disorder, macular edema, which sometimes occurs alongside it, can also obscure your central visual field. This swelling of the macular tissue can respond to any of several treatment methods, depending on the underlying cause — and Elman Retina Group can provide those treatments.
Understanding Macular Edema
The macula may be a small part of the retina, but it performs a big role in good eyesight. This area is responsible for receiving visual data related to your center of vision — that all-important zone you use to read write, watch movies, focus on objects directly in front of you and identify faces. Macular edema is a condition in which bleeding underneath the retina causes the macula to swell up. The swelling interferes with its ability to do its job, leaving with with blurred central vision. Macular edema can be present in one or both eyes.
Causes and Symptoms
The blood vessel leakage that produces macular edema is most commonly associated with a condition called diabetic retinopathy. Elevated blood sugar can damage blood vessel walls, allowing fluids to leak into the macular tissues. The “wet” form of age-related macular degeneration (AMD) can also cause macular edema due to the proliferation of new, fragile blood vessels which are prone to leakage. Other underlying health issues can sometimes lead to macular edema. These may include:
- Inflammatory diseases such as uveitis, cytomegalovirus infection, toxoplasmosis or sarcodoisis
- Complications from recent eye surgery
- Blood vessel blockage due to hypertension, atherosclerosis or glaucoma
Available Treatments for Macular Edema
Treatment of macular edema usually requires treatment of whatever underlying condition is encouraging the blood leakage. If you suffer from diabetes, for example, it is critical for you and your primary health provider to work on normalizing your blood sugar levels. If an inflammatory disorder is at work, our ophthalmology team may prescribe strong anti-inflammatory medications. These usually take the form of corticosteroid eye drops or injections. Severe cases may call for the implantation of continuous-release corticosteroids in or near the eye.
If an overgrowth of leaky blood vessels is causing your macular edema, anti-VGEF injections can help combat this trend. We can numb the eye with an anesthetic and then inject it with drugs that inhibit a particular substance called VEGF (vascular endothelial growth factor), a critical factor in blood vessel formation.
If the vitreous humor that fills the eyeball is pulling on the macula in a manner that creates macular edema, or if it is clouded with blood from blood vessel leakage, a vitrectomy may be in order. This procedure removes the vitreous humor entirely, replacing it with saline solution.
Macular Edema FAQs
How is macular edema diagnosed?
 Our retinal specialists at Elman Retina Group can diagnose macular edema during comprehensive eye exams. The eyes are dilated during these exams to widen the pupil for a detailed view of the retina lining the back of the eye. One of our board-certified ophthalmologists will ask about your medical history, lifestyle habits, and other questions to determine your risk factors for eye disease. You may be asked to look at an Amsler grid to search for areas in your field of vision that are dark, wavy, or missing. Dark areas or wavy lines on the grid sheet can indicate macular edema.
Our retinal specialists at Elman Retina Group can diagnose macular edema during comprehensive eye exams. The eyes are dilated during these exams to widen the pupil for a detailed view of the retina lining the back of the eye. One of our board-certified ophthalmologists will ask about your medical history, lifestyle habits, and other questions to determine your risk factors for eye disease. You may be asked to look at an Amsler grid to search for areas in your field of vision that are dark, wavy, or missing. Dark areas or wavy lines on the grid sheet can indicate macular edema.
If our ophthalmologists suspect macular edema, they may take images of the retina and other parts of your inner eye using a special machine for optical coherence tomography (OCT). Our specialists may also perform a fluorescein angiogram, which involves injecting a special dye into your bloodstream to see how it travels from the arm to the eye. A camera captures photos of how the dye moves through the retinal blood vessels. The images from these tests help our eye doctors identify signs of swelling or macular damage.
What are the risk factors for macular edema?
People who are overweight or obese may be more likely to experience macular edema. High blood pressure, smoking, and a history of retinal detachment increase your odds. Women who had complications during pregnancy and childbirth can develop macular edema. Previous eye surgery or eye trauma and inflammatory conditions, such as uveitis and sarcoidosis, are additional risk factors.
Natural aging can lead to age-related macular degeneration (AMD or ARMD), which damages the macula and causes irreparable central vision loss. People with blood vessel diseases, including vein occlusions or blockages, are also at risk for macular edema.
One of the most significant risk factors for macular edema is diabetes. Diabetes is a metabolic condition that causes high blood sugar (blood glucose) levels. Long-term diabetes or uncontrolled blood glucose can damage the retina, causing diabetic retinopathy or diabetic macular edema.
How does diabetes lead to macular edema?
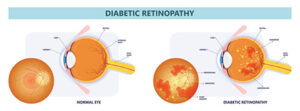 Many patients with diabetes develop eye complications around five to 10 years after their diagnosis. However, uncontrolled blood sugar can cause eye damage and vision loss before then. Too much glucose in the blood damages the retina over time, causing blood vessels around the light-sensitive tissue to swell (diabetic macular edema) and leak fluid or blood that seeps into the retina (diabetic retinopathy). As the retina swells, patients may have impaired vision or blindness in severe cases.
Many patients with diabetes develop eye complications around five to 10 years after their diagnosis. However, uncontrolled blood sugar can cause eye damage and vision loss before then. Too much glucose in the blood damages the retina over time, causing blood vessels around the light-sensitive tissue to swell (diabetic macular edema) and leak fluid or blood that seeps into the retina (diabetic retinopathy). As the retina swells, patients may have impaired vision or blindness in severe cases.
Advanced stages of diabetic retinopathy cause new, abnormal vessels to form and leak, furthering the cycle and vision loss. Early diagnosis and prompt treatment are crucial to stalling the eye disease and preserving vision.
Can macular edema be prevented?
Regular eye exams are the best way to avoid permanent macular damage. Anyone with diabetes or other risk factors should have annual dilated eye exams and schedule an appointment if they notice vision changes or warning signs of the condition. If you have a family history of eye disease or a genetic disorder that affects the macula, you may need annual exams to catch changes early.
Macular edema linked to previous eye surgery, such as cataract removal, may be reduced or prevented using nonsteroidal anti-inflammatory (NSAID) eye drops. Our eye doctors may recommend NSAID eye drops along with steroid eye drops after eye surgery to reduce the risk of macular edema.
What are the early signs of macular edema?
 Macular edema often develops gradually, making early detection difficult without regular eye exams. Initial symptoms may include mild blurriness in the central vision, difficulty reading or recognizing faces, and distortion where straight lines appear wavy. Some individuals notice that colors look duller or washed out. As fluid accumulates in the macula, vision loss can worsen, making early intervention crucial.
Macular edema often develops gradually, making early detection difficult without regular eye exams. Initial symptoms may include mild blurriness in the central vision, difficulty reading or recognizing faces, and distortion where straight lines appear wavy. Some individuals notice that colors look duller or washed out. As fluid accumulates in the macula, vision loss can worsen, making early intervention crucial.
Can macular edema lead to permanent vision loss?
If left untreated, macular edema can result in irreversible damage to the retina and permanent central vision loss. The swelling can distort the light-sensitive cells in the macula, leading to progressive vision impairment. However, with timely diagnosis and appropriate treatment — such as anti-VEGF injections, corticosteroids, or laser therapy — many patients can maintain or even improve their vision. Regular follow-up appointments are essential to monitor for recurrence and prevent long-term damage.
How is macular edema different from macular degeneration?
Although both conditions affect the macula, they differ in causes and progression. Macular edema results from fluid leakage due to abnormal or damaged blood vessels, often linked to diabetic retinopathy, retinal vein occlusion, or inflammation. It can develop suddenly and is treatable if addressed early. Macular degeneration, particularly age-related macular degeneration (AMD), is a degenerative condition that leads to the gradual breakdown of macular cells, affecting central vision over time. Unlike macular edema, AMD is not caused by fluid buildup but by the deterioration of retinal tissue or the growth of abnormal blood vessels beneath the macula. While treatment can slow its progression, there is no cure for AMD.
What are lifestyle changes to support macular health?
 Healthy lifestyle choices can play a significant role in supporting macular function and reducing the risk of worsening macular edema. A diet rich in leafy greens, colorful fruits, and foods high in omega-3 fatty acids — such as salmon and flaxseeds — helps provide essential nutrients like lutein, zeaxanthin, and vitamins C and E. Maintaining healthy blood sugar and blood pressure levels is also crucial, particularly for those with diabetes or vascular conditions, as high levels can exacerbate retinal swelling. Regular exercise improves circulation to the eyes, while avoiding smoking and excessive alcohol consumption can help protect retinal blood vessels. Wearing sunglasses with UV protection minimizes light-related damage, and staying consistent with prescribed medications and eye exams ensures early detection of any changes.
Healthy lifestyle choices can play a significant role in supporting macular function and reducing the risk of worsening macular edema. A diet rich in leafy greens, colorful fruits, and foods high in omega-3 fatty acids — such as salmon and flaxseeds — helps provide essential nutrients like lutein, zeaxanthin, and vitamins C and E. Maintaining healthy blood sugar and blood pressure levels is also crucial, particularly for those with diabetes or vascular conditions, as high levels can exacerbate retinal swelling. Regular exercise improves circulation to the eyes, while avoiding smoking and excessive alcohol consumption can help protect retinal blood vessels. Wearing sunglasses with UV protection minimizes light-related damage, and staying consistent with prescribed medications and eye exams ensures early detection of any changes.
What can you expect after macular edema treatment?
The prognosis for macular edema depends on the underlying cause, severity, and how quickly treatment is initiated. Many patients experience significant vision improvement with therapies such as anti-VEGF injections, corticosteroids, or laser treatments. However, macular edema may require ongoing management, as some individuals are prone to recurrence. Regular monitoring allows our doctors to adjust treatment as needed. While some vision changes may persist, early intervention greatly increases the likelihood of preserving functional eyesight. Patients should maintain a proactive approach to eye health by following medical recommendations, attending follow-up visits, and making necessary lifestyle adjustments to protect their vision long-term for the long term.
Elman Retina Group Is Ready to Help
Macular edema can be treated — and the sooner you arrange for it, the brighter your ocular future will look. Call the Rosedale, Glen Burnie or Pikesville office of Elman Retina Group to schedule an evaluation and treatment!



